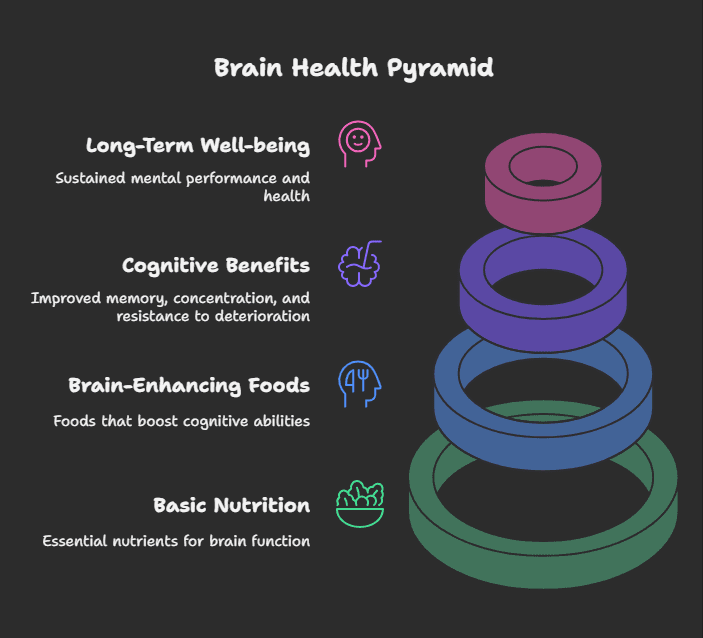
Do you think your brain could use a little work? You might have trouble focusing during a long day at work, can’t remember names anymore, or just want to keep your mind sharp as you get older. Don’t worry, you’re not alone! It’s never been more important to improve cognitive function because of how busy we are. The good news is that one of the best things you can do for your brain is right on your plate. Welcome to the interesting world of brain-boosting foods. These tasty, nutrient-rich foods can help feed your mind, boost your memory, and help you focus. This article will look at the top 10 foods that are known to be good for your brain and explain the science behind how they work.
We often think about diet when we want to lose weight or have a healthy heart, but there is a deep connection between what we eat and how we feel. Even though our brain only makes up about 2% of our total weight, it burns about 20% of the calories we eat each day! It’s a hungry organ that needs a steady supply of certain nutrients to work well. It’s not about taking a magic pill or becoming a genius overnight; it’s about giving your brain the building blocks it needs to stay healthy, strong, and perform at its best all the time. So, let’s go on this food journey to get a sharper, healthier mind!
Why Does What We Eat Matter So Much for Our Brain?
Before we get into the particular foods, let’s take a quick look at why nutrition is so important to brain health.
- Energy Supply: As noted, the brain requires a great deal of energy, and it gets it mainly from glucose (carbohydrates). But the quality of carbohydrates makes a difference. Complex carbs offer a slow release, whereas simple sugars lead to energy highs and lows, influencing concentration and mood.
- Building Blocks: Fats, especially Omega-3 fatty acids, are essential structural building blocks of brain cell membranes. They ensure fluidity and act as facilitators for neuron-to-neuron communication. Proteins offer amino acids, which are the building blocks of neurotransmitters – chemical messengers that control mood, sleep, focus, and more.
- Protection: The brain is very vulnerable to oxidative stress, a process induced by unstable molecules known as free radicals that have the potential to harm cells. Antioxidants, which are present in high amounts in most plant foods, neutralize free radicals, shielding brain cells from harm and inflammation.
- Blood Flow: Proper circulation is essential to bring oxygen and nutrients to the brain. Some foods can promote healthy blood vessels and enhance blood flow, enhancing overall cognitive function.
- Inflammation Control: Ongoing inflammation has been associated with many health problems, including cognitive impairment. Many of the nutrients in whole foods possess anti-inflammatory effects that can protect the brain.
In essence, a diet rich in the right nutrients supports the brain’s structure, fuels its activity, shields it from harm, and provides it with what it requires through healthful blood flow. Now, let’s get to the superstars – the top 10 brain-boosting foods.
The Top 10 Brain-Boosting Foods List
Below are ten great foods renowned for their beneficial effects on cognitive wellness:
1. Fatty Fish: The Omega-3 Powerhouse
(Examples: Salmon, Mackerel, Trout, Herring, Sardines)
Why it’s a Brain Booster: Fatty fish are teeming with omega-3 fatty acids, specifically docosahexaenoic acid (DHA) and eicosapentaenoic acid (EPA). Your brain contains approximately 60% fat, and half of that fat consists of omega-3s, mostly DHA.
How it Works:
- Structural Component: DHA is necessary for constructing and maintaining the structure of brain cell membranes (neurons). Healthy membranes are important for the transmission of nerve signals.
- Anti-inflammatory: Omega-3s possess strong anti-inflammatory properties, which can potentially shield the brain from conditions associated with chronic inflammation.
- Neuroprotection: Research indicates that omega-3s may boost blood flow to the brain, promote the development of new nerve cells, and, possibly, reduce levels of beta-amyloid, the protein that aggregates to form clumpy proteins in the brains of individuals with Alzheimer’s disease.
Cognitive Benefits: Associated with enhanced memory, enhanced learning abilities, improved mood, and reduced risk of age-related cognitive impairment and dementia.
How to Add It: Shoot for at least two servings of fatty fish a week. Grill, bake, or steam it. If you don’t like fish, try a high-quality fish oil or algae-based omega-3 supplement (talk to your doctor first).
2. Blueberries: The Antioxidant Champions
(Also include other intensely colored berries such as blackberries, raspberries, strawberries)
Why it’s a Brain Booster: Blueberries are full of antioxidants, specifically a class known as flavonoids, and anthocyanins are the heroes behind their intense blue/purple color.
How it Works:
- Fights Oxidative Stress: Anthocyanins and other antioxidants kill off destructive free radicals that will destroy brain cells and lead to aging and neurodegenerative diseases.
- Lowers Inflammation: These substances also contain anti-inflammatory properties, further safeguarding brain tissue.
- Enhances Cell Signaling: Blueberry compounds are found to be accumulated in the brain and facilitate enhanced communication between cells in the brain. They have the potential to enhance neuroplasticity – the adaptability and flexibility of the brain
Cognitive Benefits: The studies attribute the consumption of blueberries to postponing short-term memory loss, enhancing motor abilities, and lesser the risk of cognitive decline due to age.
How to Incorporate It: Take a handful of fresh or frozen. Use them as add-ins to smoothies, yogurt, oatmeal, salads, or enjoy as a quick snack.
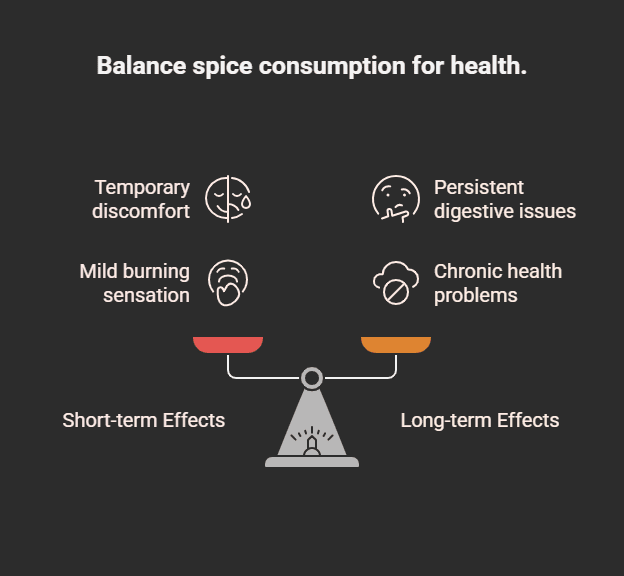
3. Turmeric: The Mind-Boosting Golden Spice
(Active Constituent: Curcumin)
Why it’s a Brain Power Boost: This bright yellow spice found in curry powder has a mighty compound, curcumin.
How it Functions:
- Powerful Anti-inflammatory & Antioxidant: Curcumin acts directly against inflammation and oxidative stress, both of which are central to brain aging and neurodegenerative diseases.
- Crosses the Blood-Brain Barrier: Importantly, curcumin can cross the blood-brain barrier, so it can act directly within the brain.
- Boosts BDNF: Curcumin may increase levels of Brain-Derived Neurotrophic Factor (BDNF), a growth hormone that functions in the brain, helping neurons survive, grow, and form new connections. Low BDNF levels are linked to depression and Alzheimer’s.
- May Clear Amyloid Plaques: Some research suggests curcumin might help clear the amyloid plaques characteristic of Alzheimer’s disease
.Cognitive Benefits: Associated with enhanced memory, fewer depressive symptoms, and possibly slowing age-related mental decline.
How to Incorporate It: Mix turmeric into curries, soups, stews, rice, or scrambled eggs. Prepare “golden milk” (turmeric latte). Mix with black pepper (which has piperine) to greatly boost curcumin absorption.
4. Broccoli: The Green Guardian
(Also, other cruciferous vegetables such as cauliflower, kale, and Brussels sprouts)
Why it’s a Brain Booster: Broccoli is a nutrient powerhouse, full of antioxidants and containing a high amount of Vitamin K.
How it Works:
- Vitamin K: This fat-soluble vitamin is necessary for creating sphingolipids, a form of fat tightly compacted into brain cell membranes. Greater Vitamin K consumption is associated with improved memory and cognitive functioning.
- Antioxidant & Anti-inflammatory: Broccoli is rich in various powerful antioxidant and anti-inflammatory agents, some of which, like sulforaphane, have cell-damage-protecting effects. Sulforaphane could also produce neuroprotective effects.
- Vitamin C: Rich in Vitamin C as well, another key antioxidant.
Cognitive Benefits: Maintains the formation of memories, shields cells from oxidative damage, and promotes maintenance of general brain health.
How to Add It: Steam, roast, stir-fry, or have it raw with dip. Mix it into soups, stews, pasta, or omelets. Steaming saves more nutrients than boiling.
5. Pumpkin Seeds: Small Seeds, Big Minerals
Also pepitas)
Why it’s a Brain Booster: These tiny seeds are very dense in several micronutrients essential for brain function: zinc, magnesium, copper, and iron.
How it Works:
- Zinc: Essential for transmitting nerve signals and plays a role in memory, thinking. It is associated with neurological diseases such as Alzheimer’s and depression.
- Magnesium: Needed to learn and memorize. There is an association between low levels of magnesium and migraines, depression, and epilepsy. It facilitates nerve transmission, neuromuscular conduction.
- Copper: Copper is utilized by your brain to assist in controlling nerve impulses. A deficiency of copper may promote neurodegenerative disorders.
- Iron: Iron deficiency has been described in terms of “brain fog” and impaired cognition, since iron is essential for oxygen delivery to the brain as well as the synthesis of neurotransmitters.
Cognitive Benefits: Facilitates nerve conduction, memory, learning, and guards against neurological disorders associated with mineral deficiencies.
How to Include It: Snack on them raw or toasted. Sprinkle them over salad, yogurt, oatmeal, or soups. Mix into homemade granola or trail mix.
6. Dark Chocolate & Cocoa Powder: A Delicious Dose of Flavonoids
(Look for 70% cocoa solids or higher)
Why it’s a Brain Booster: Dark chocolate and cocoa powder are rich in brain-friendly ingredients, such as flavonoids, caffeine, and antioxidants.
How it Works:
- Flavonoids: These plant compounds build up in parts of the brain that are used for learning and memory. They are powerful antioxidants and anti-inflammatories. Studies indicate they can increase neuroplasticity and increase blood supply to the brain.
- Caffeine & Theobromine: Natural stimulants that can improve alertness and mood in the short term.
- Improved Blood Flow: Flavonoids can cause relaxation of blood vessels, possibly improving blood flow to the brain
.Cognitive Benefits: Can improve memory, enhance concentration and attention span, elevate mood, and ward off age-related cognitive decline. The more cocoa, the better (and less sugar).
How to Incorporate It: Savor a small piece (about 1 ounce) of dark chocolate (70 %+) as a treat. Add unsweetened cocoa powder to smoothies or healthy baking. Use in moderation because of calories and caffeine.
7. Nuts: Nature’s Brain Food Nuggets
(Especially Walnuts, Almonds, Hazelnuts)
Why it’s a Brain Booster: Nuts are rich in healthy fats, antioxidants (such as Vitamin E), and other useful nutrients.
How it Works
- Healthy Fats: Supply energy and maintain brain cell structure (like fatty fish, although plant-based omega-3s such as ALA in walnuts require conversion in the body, which is less effective than receiving DHA/EPA directly).
- Vitamin E: A powerful antioxidant that guards cell membranes against free radical damage. Greater Vitamin E intake is linked to reduced cognitive slowdown.
- Other Nutrients: Nuts are also sources of minerals and B vitamins useful to the brain. Walnuts are especially emphasized for containing more ALA omega-3 fatty acids and special antioxidants.
Cognitive Advantages: Attributed to improved overall cognition, enhanced memory, and a reduction in age-related cognitive impairment. Frequent nut eating has been linked to more acute thinking later in life.
How to Incorporate It: A small serving of assorted nuts is an excellent snack. Sprinkle chopped nuts over salads, oatmeal, yogurt, or stir-fries. Spread nut butter on whole-grain bread or fruit.
8. Oranges (and other Vitamin C foods)
(Examples: Bell Peppers, Guava, Kiwi, Strawberries, Tomatoes)
Why it’s a Brain Booster: Oranges are renowned for their Vitamin C content, a potent antioxidant that is vital for brain function.
How it Works:
- Powerful Antioxidant: Vitamin C fights off free radicals that can harm brain cells. It is crucial in preventing mental decline.
- Neurotransmitter Synthesis: It’s responsible for the production of neurotransmitters such as dopamine and norepinephrine, which influence mood and cognitive function.
- Supports Overall Brain Health: Having sufficient Vitamin C levels is important as we get older. Research indicates increased blood levels of Vitamin C are linked to improvements in tasks requiring attention, memory, focus, and decision speed.
Cognitive Benefits: Prevents age-related mental decline, supports neurotransmitter function, and guards against oxidative stress.
How to Include It: Eat one medium orange to get nearly your entire recommended daily amount of Vitamin C. Enjoy other Vitamin C-rich fruits and vegetables daily. Eating the whole fruit is better than juice due to the fiber content.
9. Eggs: Choline Champions
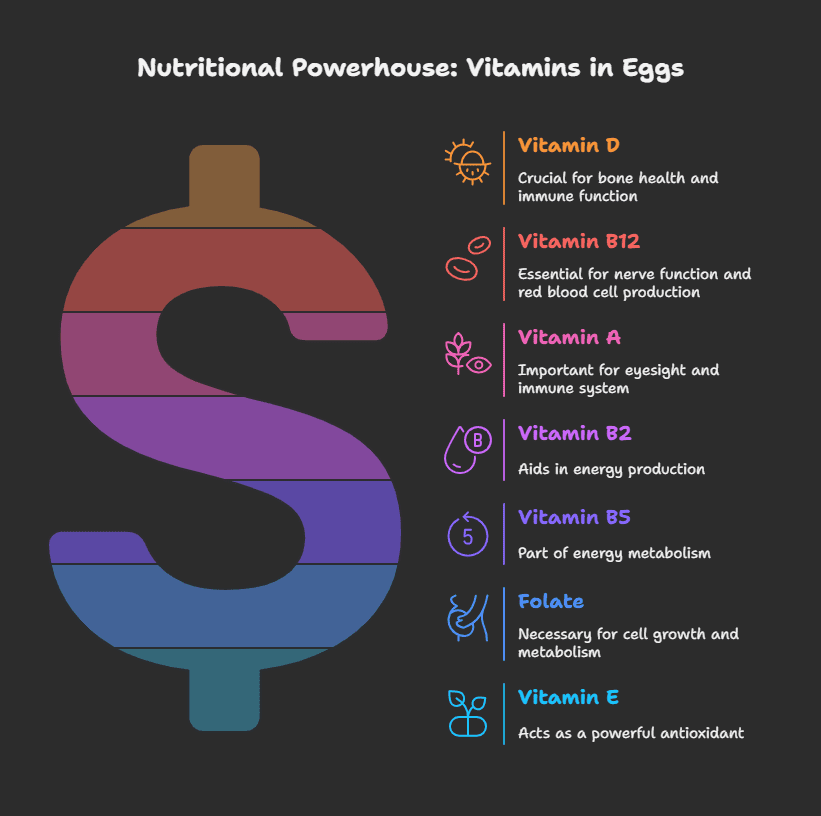
Why it’s a Brain Booster: Eggs are a great source of various nutrients linked to brain functioning, such as B vitamins (B6, B12, folate) and, not insignificantly, choline.
How it Works:
- Choline: Your body employs choline to produce acetylcholine, an important neurotransmitter that is necessary for memory, mood control, and muscle contraction. Increased choline consumption has been associated with improved memory and cognitive functioning. Egg yolks are among the richest sources of choline.
- B Vitamins (Folate & B12): These vitamins contribute to brain health by helping slow down cognitive decline. They do so partially by assisting with the breakdown of homocysteine, an amino acid whose elevated levels have been found to increase the risk of dementia and Alzheimer’s disease.
- B6: Also contributes to the synthesis of important neurotransmitters.
Cognitive Benefits: Supports memory formation, mood regulation, and helps prevent age-related cognitive decline and brain shrinkage.
How to Include It: Enjoy eggs boiled, poached, scrambled, or in omelets. They are versatile and can be part of breakfast, lunch, or dinner.
10. Green Tea: Calm Focus in a Cup
Why it’s a Brain Booster: Green tea offers a unique combination of compounds that benefit the brain.
How it Works:
- L-Theanine: An amino acid present in green tea that can cross the blood-brain barrier. It enhances the activity of the inhibitory neurotransmitter GABA, which has a calming effect. It enhances dopamine and alpha wave activity in the brain, inducing relaxation without causing drowsiness and enhancing concentration.
- EGCG (Epigallocatechin Gallate): A highly effective polyphenol and antioxidant that has antioxidant effects in brain cells and can have neuroprotective properties.
- Caffeine: Gives a subtle increase in alertness and performance (less jittery than coffee for many because of L-theanine). The combination of L-theanine and caffeine is especially useful for enhancing attention and concentration.
Cognitive Benefits: Increases alertness, concentration, memory, and working memory. Reduces anxiety and induces relaxation. Shields against neurodegenerative diseases.
How to Incorporate It: Steep green tea with water that is not boiling (about 80°C or 175°F) to prevent bitterness. Drink 1-3 cups daily. Matcha, a powdered green tea, provides a more concentrated amount of these health-promoting compounds.
Developing a Diet Full of Brain-Enhancing Foods: Beyond the Top 10
While concentrating on these top 10 brain foods is a good beginning, keep in mind that overall eating habits are most important. Here are a few additional suggestions
- Hydration: Your brain contains approximately 75% water! Dehydration can rapidly impair concentration, memory, leading to brain fog. Drink lots of water during the day.
- Gut Health: The gut-brain axis is a popular topic for a reason. A balanced gut microbiome (the collection of bacteria in your intestines) affects brain health and mood. Add prebiotic fiber (from vegetables, fruits, and whole grains) and probiotic foods (such as yogurt, kefir, and sauerkraut) to maintain gut health.
- Limit Harmful Foods: Equally important as adding healthy foods is restricting those that can hurt brain health. These include:
Sugary beverages and highly refined sugars can cause energy crashes, inflammation, and weakened memory.
Refined carbs (white bread, pasta, pastry – same effects as sugar).
Trans fats (in some packaged foods) are associated with cognitive loss.
Highly processed foods (usually high in sugar, bad fats, and low in nutrients).
- Variety is Key: Don’t just stick to these 10 foods. Opt for a varied diet with plenty of various fruits, vegetables, whole grains, lean proteins, and healthy fats to maximize the intake of a wide variety of nutrients. The Mediterranean dietary pattern, for example, is consistently associated with improved brain health.
- Combine with Lifestyle: Keep in mind that diet works synergistically with other health behaviors. Regular physical exercise, sufficient sleep (7-9 hours), stress management, and ongoing learning are all critical parts of keeping your brain sharp and healthy.
Conclusion: Feed Your Brain!
Your brain controls everything you think, feel, and do, so it’s the most important thing you have.
One of the best things you can do for your mental health and cognitive performance in the future is to feed it the right foods. Adding foods that are good for your brain, like fatty fish, blueberries, turmeric, broccoli, pumpkin seeds, dark chocolate, nuts, oranges, eggs, and green tea, to your daily diet can give you the nutrients you need to work at your best, remember things, concentrate, and stay healthy. Not perfect, but better. Start by adding one or two of these foods to your meals each week. Over time, small, gradual changes can lead to big benefits. So, eat well, stay interested, and take the trip to a healthier, sharper you, one tasty bite at a time!