Let’s talk about something very personal and, for many, very upsetting: hair loss and alopecia. For a lot of people, their hair is a big part of who they are, how they feel about themselves, and how confident they are. It can be scary to find more hair than usual on your brush, in the drain, or in areas that are getting thinner. But you aren’t the only one. Alopecia, or hair loss, happens to millions of men and women around the world for a lot of different reasons.
The goal of this article is to make alopecia hair loss less mysterious. We’ll talk about the normal cycle of hair growth, the different types of alopecia, the usual causes of hair loss, how it’s diagnosed, and, most importantly, the different ways to treat it and deal with it that are available right now. The first step to finding effective solutions and getting some control over your hair loss is to understand the “why” and “what” of it.
The Life Cycle of Your Hair: A Quick Primer
Before we discuss why hair loss occurs, it’s helpful to know how hair grows normally. Every hair follicle on your head works separately, going through three phases of existence:
- Anagen (Growth Phase): This is the proliferative growth phase. Hair follicles develop hair fibre, and the hair shaft elongates. This phase lasts anywhere from 2 to 7 years and determines the length of your hair. At any time, around 85-90% of your scalp hairs are in the anagen phase.
- Catagen (Transition Phase): A Brief transitional phase that lasts around 2-3 weeks. Hair growth ceases, and the hair follicle becomes slightly smaller, breaking away from its blood supply. Only approximately 1-2% of your hair is in this phase.
- Telogen (Resting Phase): The follicle rests for approximately 3-4 months. The previous hair stays in position, but it’s no longer growing. This resting hair is eventually lost (usually when you brush or shampoo your hair) as a new anagen hair starts to grow underneath it, displacing it. Approximately 10-15% of your scalp hairs are usually in the telogen phase.
You would typically lose around 50 to 100 telogen hairs daily. This is completely normal and typically unnoticed since new hairs continuously begin their anagen stage. Hair loss alopecia results if this process is interrupted – either by additional hairs entering the telogen stage too early, the anagen stage decreasing, or the follicle damaged or destroyed.
What Exactly is Alopecia?
Alopecia is just the technical name for loss of hair, without regard to cause or distribution. It is not one disease but a symptom that may be due to several underlying diseases or causes. It can occur in many forms:
- Thinning of hair on top of the head (most common form).
- Circular or patchy baldness.
- Sudden shedding and loosening of hair.
- Hair loss on the entire body.
- Hair loss with scaling or redness on the scalp.
It may be temporary or permanent, be limited to the scalp or the whole body, and happen at any age, but it gets more prevalent as we age.
Unpacking the Various Types of Hair Loss: Alopecia
Alopecia is not a condition that fits all. Knowing which particular type you may be suffering from is the first step to identifying the best solution. Here are some of the most prevalent types:
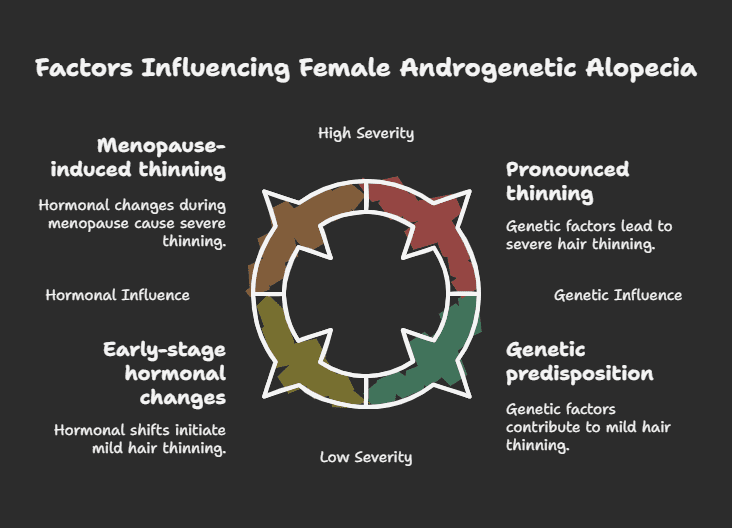
What it is: This is the most common form of hair loss, commonly called male-pattern baldness or female-pattern baldness. It’s highly associated with genetics and the effect of androgens (male hormones), especially dihydrotestosterone (DHT).
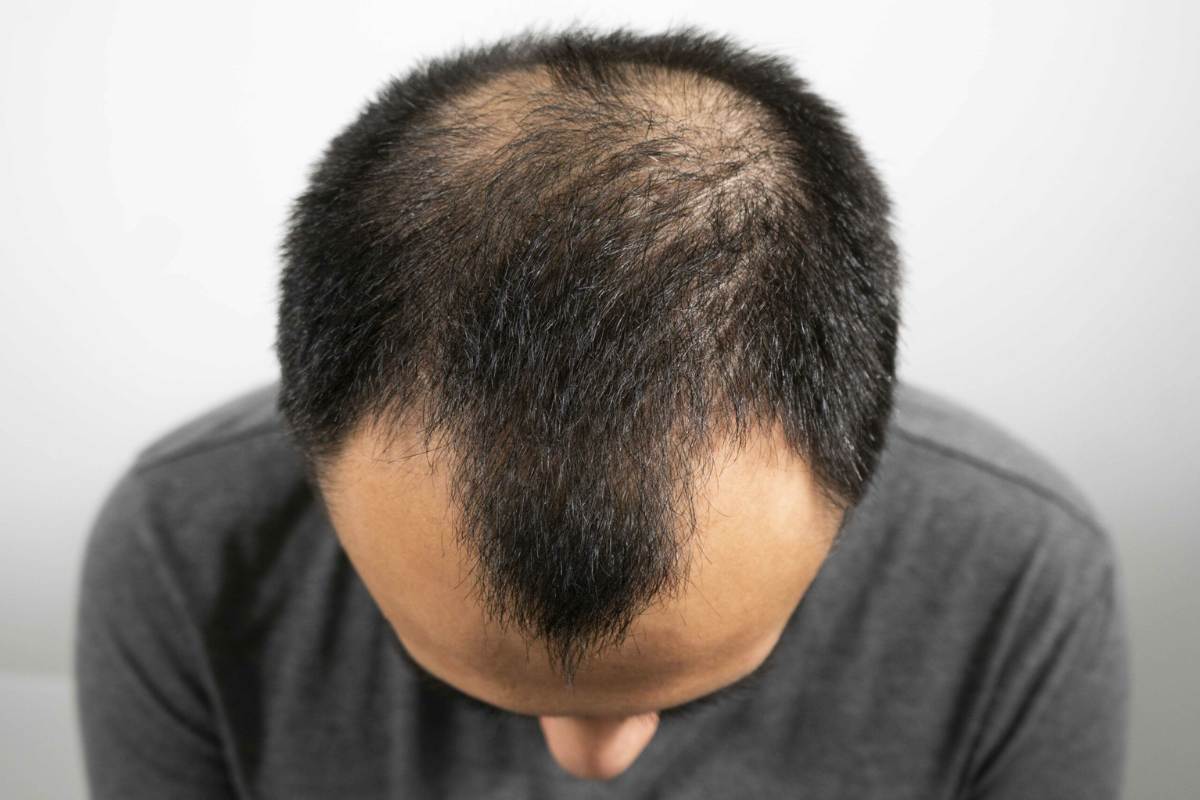
How it looks: In men, it typically starts with a receding hairline and thinning at the crown, potentially progressing to partial or complete baldness. In women, it usually presents as diffuse thinning over the entire scalp, particularly at the part line, while the frontal hairline is often preserved. Complete baldness is rare in women.
Mechanism: Hair follicles that are responsive to DHT slowly shrink (miniaturize). This decreases the anagen (growth) phase and prolongs the telogen (resting) phase, leading to thinner, shorter hairs until finally, growth is completely halted.
Alopecia Areata:
Androgenetic Alopecia (Pattern Hair Loss):
- What it is: An autoimmune disorder in which the body’s immune system mistakenly attacks healthy hair follicles, creating inflammation and hair loss. The cause is unknown, but genetics and environmental factors are suspected to be involved.
- How it appears: Involves abrupt onset of smooth, circular, coin-shaped bald patches on the scalp or body hair-bearing areas (beard, eyebrows). It may be one or more patches (Alopecia Areata monolocularis/multilocularis) or complete loss of scalp hair (Alopecia Totalis) or all body hair (Alopecia Universalis).
- Prognosis: The pattern is unpredictable. The hair will regrow on its own, sometimes a different colour or texture at first, or the loss can continue or recur.
Telogen Effluvium (TE):
What it is: A form of diffuse hair loss that results when a major stressor forces a large number of hair follicles too early into the telogen (resting/shedding) phase.
- Triggers: General triggers are major physical stress (surgery, high fever, childbirth, serious illness such as COVID-19), extreme emotional stress, extreme weight loss, nutritional deficiencies (particularly iron), thyroid issues, and some medications.
- How it looks: Presented by increased shedding throughout the entire scalp, commonly observed 2-4 months following the trigger event. It usually causes appreciable thinning but not actual bald patches.
- Prognosis: Typically temporary. Once the causative underlying factor is reversed or eliminated, the hair growth cycle usually returns to normal within 6-9 months, although healing may seem to be slow. Chronic Telogen Effluvium is possible, but it is not as prevalent
Anagen Effluvium:
- .What it is: Sudden and diffuse loss of hair due to damage to hair follicles during the anagen (growing) phase.
- Causes: Most frequently linked to chemotherapy or head radiation therapy, which affects quickly dividing cells, including hair follicles. Certain poisons may also cause it.
- How it appears: Sudden loss of most scalp hair shortly after the causative agent has been encountered.
- Prognosis: Hair generally returns after the treatment (such as chemotherapy) has been discontinued, as the follicles are injured but not usually killed
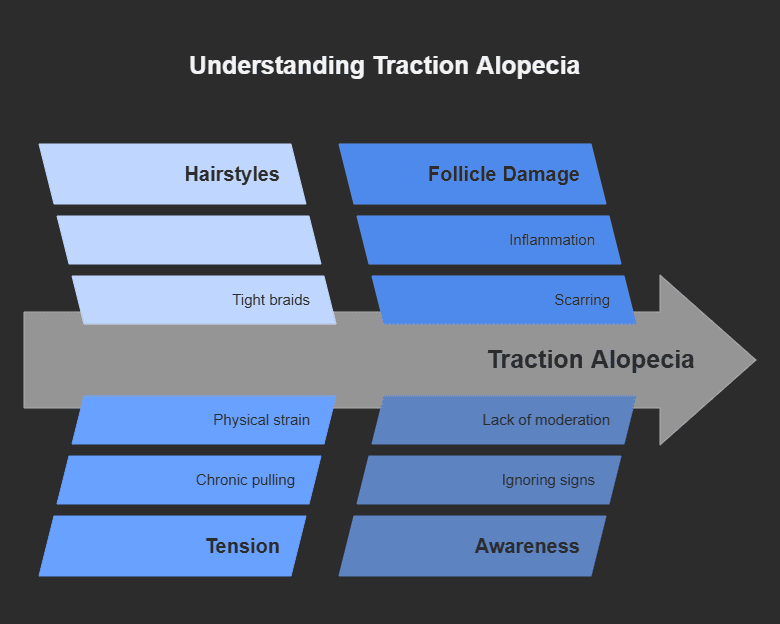
Traction Alopecia:
- .What it is: Hair loss due to repeated or constant tension on the hair follicles.
- Causes: Specific hairstyles that draw on the hair tightly, including tight ponytails, braids, cornrows, dreadlocks, and hair extensions, particularly when worn for extended periods. Heat and chemical treatment can cause the weakening of the hair, which makes it vulnerable.
- How it appears: Usually involves the hairline (frontal and temporal regions) or regions subject to chronic tension. At first, it may appear as minute bumps near follicles (folliculitis), then breakage and thinning of the hair.
- Prognosis: Curable if discovered early and the tension is relieved. Chronic, prolonged traction can, however, cause permanent follicle damage and scarring and result in irreparable loss of hair.
Cicatricial Alopecia (Scarring Alopecia):
- What it is: A collection of uncommon inflammatory conditions that destroy the hair follicle and replace it with scar tissue. This results in permanent hair loss.
- Causes: May be caused by many conditions, such as Lichen Planopilaris, Frontal Fibrosing Alopecia, Central Centrifugal Cicatricial Alopecia (CCCA), Discoid Lupus Erythematosus, and Folliculitis Decalvans. The cause usually has an underlying inflammation targeted at the top of the hair follicle.
- How it appears: Dependent on the particular type, but can include patchy hair loss with associated signs such as itching, burning, pain, redness, scaling, or pustules of the scalp. The scarred scalp skin can appear smooth and shiny.
- Prognosis: Permanent loss of hair in scarring. Treatment is directed towards halting the inflammation and preventing further hair loss
What Causes and Raise the Risk of Hair Loss Alopecia?
.Knowledge of the possible triggers is essential for prevention and treatment. Important causes of hair loss, alopecia, are:
Genetics (Heredity): The most prevalent cause of pattern hair loss (Androgenetic Alopecia). If your parents or immediate relatives suffered from hair loss, your risk is increased.
Hormonal Changes: Changes or imbalances can lead to hair loss. This includes:
- Pregnancy and Childbirth (often causing temporary Telogen Effluvium).
- Menopause.
- Thyroid disorders (both hyperthyroidism and hypothyroidism).
- Polycystic Ovary Syndrome (PCOS).
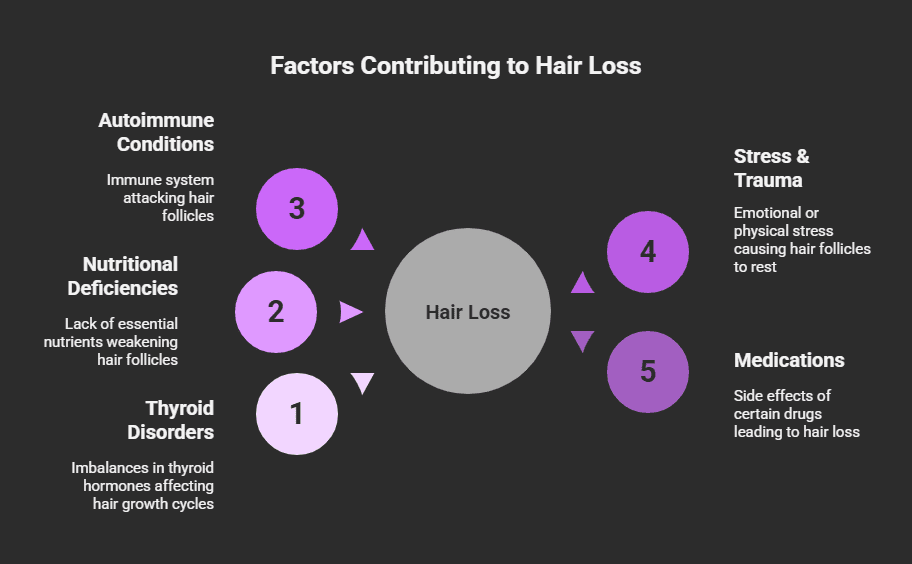
Medical Conditions:
- Autoimmune diseases (Alopecia Areata, Lupus).
- Scalp infections (like ringworm or tinea capitis).
- Skin disorders (psoriasis, seborrheic dermatitis on the scalp).
- Conditions causing nutritional deficiencies.
Medications and Treatments:
- Chemotherapy and radiation therapy.
- Certain drugs are used for arthritis, depression, heart problems, high blood pressure, and gout.
- High levels of Vitamin A.
- Birth control pills (sometimes when beginning or ceasing).
- Anabolic steroids.
Nutritional Deficiencies: Insufficiency of necessary nutrients may affect hair well-being. Iron, protein, zinc, biotin, and essential fatty acid deficiencies are commonly involved. Crash dieting or malnutrition may cause TE.
Stress: Extreme physical or emotional stress may cause Telogen Effluvium. Ongoing stress may also worsen other forms of hair loss.
Hair Care Habits and Therapies:
- Traction Alopecia due to tight hairstyles.
- Chemical damage from aggressive chemical treatments (perms, relaxers, color).
- Excessive heat use.
Age: Hair naturally will thin, and hair density can slow down as we get older, even without a distinct alopecia disorder. Follicles can simply become less efficient over time.
Getting a Diagnosis: When to See a Doctor
While a little shedding is to be expected, it’s a good idea to see a doctor or dermatologist if you experience:
- Sudden or patchy hair loss.
- Excessive overall shedding for a few weeks.
- Itching, painful, red, or scaly scalp with hair loss.
- You’re concerned about your pattern of hair loss.
- Hair loss is affecting your self-esteem.
A dermatologist specializing in hair loss (sometimes called a trichologist, though ‘trichologist’ isn’t always a regulated medical title – ensure they are a board-certified dermatologist) can help determine the cause. Diagnosis typically involves:
- Medical and Family History: Discussing your health, medications, diet, stress levels, hair care routine, and family history of hair loss.
- Physical Exam: Carefully looking at your hair loss pattern, scalp, and quality of the hair shaft. They may use a dermatoscope (a type of magnifying lens) to take a closer look at the follicles and scalp skin.
- Pull Test: Lightly tugging a short section of hair (about 40-60 hairs) to observe how many fall out with ease. A number greater than a few hairs could indicate active shedding (such as in TE).
- Blood Tests: To identify underlying conditions such as thyroid disease, iron deficiency (anemia), hormonal imbalances, or vitamin deficiencies.
- Scalp Biopsy: In a few instances, particularly if scarring alopecia or an inflammatory process is suspected, a small piece of scalp skin (typically 4mm) is taken under local anesthesia and viewed under the microscope.
Treatment Options for Hair Loss Alopecia: Finding What Works
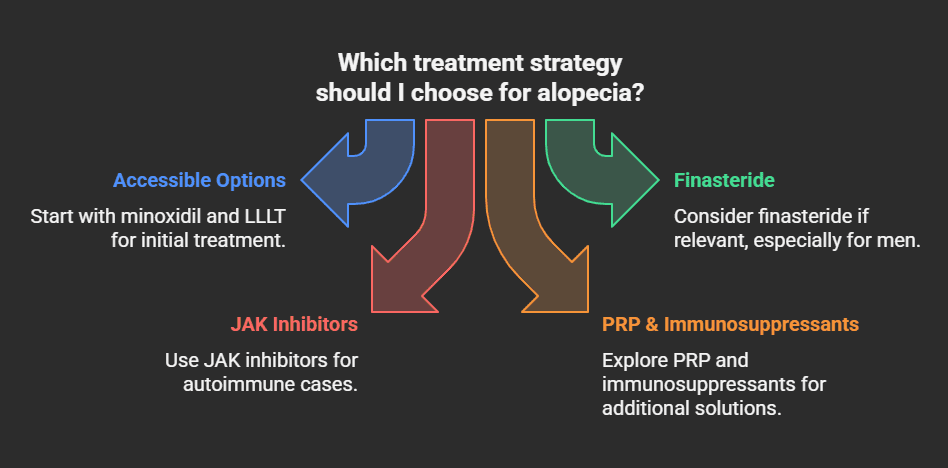
The ideal treatment largely varies with the type and reason for your alopecia hair loss. It is important to be properly diagnosed before initiating treatment. Depending on your case, the following are options that vary from medications and procedures to lifestyle modifications:
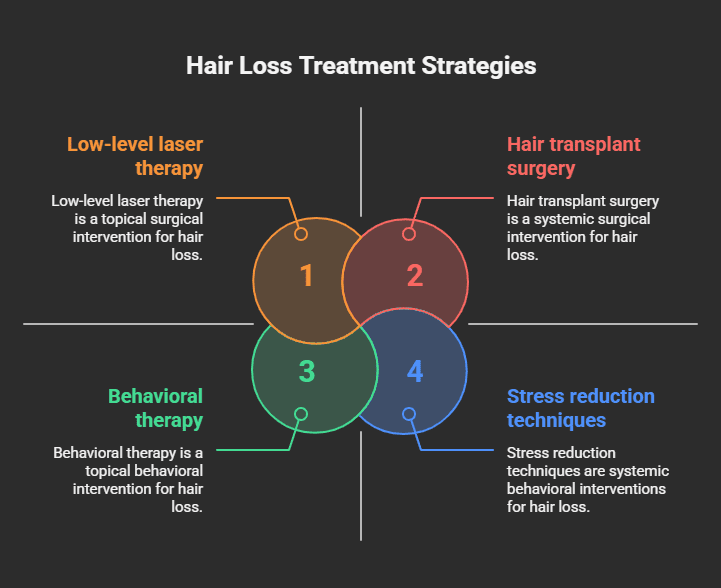
Over-the-Counter (OTC) Treatments:
- Minoxidil (Rogaine®): A topical liquid or foam put directly on the scalp. It’s FDA-approved for androgenetic alopecia in men and women and is also said to help some individuals with alopecia areata or TE. It extends the anagen phase and perhaps enlarges follicles. It doesn’t always work, needs to be used continuously to sustain results, and takes a couple of months to become effective.
Prescription Medications
- Finasteride (Propecia®): Oral medication for men with androgenetic alopecia. It is an inhibitor of the enzyme (5-alpha-reductase) that converts testosterone into DHT, the hormone causing follicle miniaturization. It is typically more effective in slowing loss and stimulating regrowth at the crown than at the hairline. Not generally used in women of childbearing age because it poses risks to the fetus if a woman were to become pregnant.
- Spironolactone: An oral drug sometimes used off-label for female pattern hair loss. It’s an anti-androgen, which counteracts the hormonal impact on hair follicles.
- Corticosteroids: To decrease inflammation in conditions such as Alopecia Areata and certain Scarring Alopecias. Can be administered as injections into the involved scalp areas, applied topically (creams/lotions), or orally (generally for extensive or severe cases, with more possible side effects).
- Other Immunosuppressants (e.g., Methotrexate, JAK inhibitors): Occasionally used for resistant or severe Alopecia Areata or some inflammatory Scarring Alopecias. These need to be monitored closely because of side effects.
- Antifungals: For fungal infection-induced hair loss, such as tinea capitis.
Medical Procedures:
- Hair Transplantation: A surgical operation by which hair follicles are transferred from a donor site (often the back or sides of the head, which are less susceptible to balding) to balding or thinning spots. Methods include Follicular Unit Transplantation (FUT or strip procedure) and Follicular Unit Extraction (FUE). Ideal for Androgenetic Alopecia or chronic Scarring Alopecia after the inflammatory process has been brought under control. The outcome is usually long-lasting but costly.
- Platelet-Rich Plasma (PRP) Therapy: Involves taking your own blood, processing it to thicken the platelets (growth factor-rich), and injecting the PRP into the scalp. It’s believed to awaken latent hair follicles and stimulate growth. Evidence continues to develop, but it’s applied to Androgenetic Alopecia and occasionally Alopecia Areata. Repeated sessions are typically required.
- Low-Level Laser Therapy (LLLT): Equipment (helmets, helmets, combs, bands) releases red light wavelengths believed to stimulate cellular function in follicles, which could extend the anagen phase and boost hair density. FDA cleared for Androgenetic Alopecia. Must use regularly over several months; success is variable.
Lifestyle and Home Remedies:
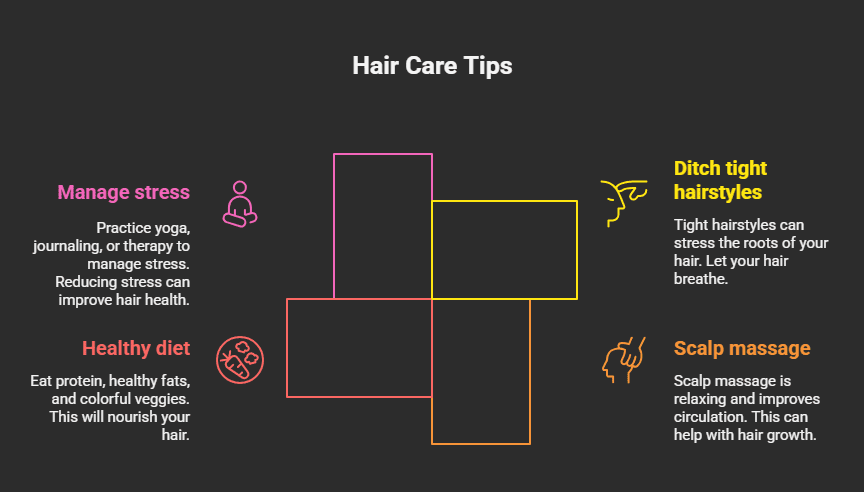
- Gentle Hair Care: Shun harsh treatments, heat, and tight styles. Use a wide-tooth comb, particularly on wet hair. Select mild shampoos.
- Balanced Diet: Take sufficient protein, iron, zinc, biotin, omega-3 fatty acids, and vitamins. Treat diagnosed nutritional deficiencies with supplements if advised by your physician.
- Stress Management: Methods such as yoga, meditation, exercise, or therapy can manage stress, possibly preventing TE or stress-induced worsening of other conditions.
- Scalp Massage: Can enhance circulation to the scalp, although strong evidence for meaningful regrowth is scarce.
Cosmetic Solutions:
- Wigs and Hairpieces: Excellent quality in synthetic or human hair, providing instant coverage and styling flexibility.
- Hair Fibers and Concealers: Sprays or powders that stick to the remaining hair, giving the illusion of thicker hair and covering thinning spots.
- Strategic Hairstyling: Thin hair can be disguised by a well-cut style. Layering or texturizing will help.
Can Hair Loss Be Prevented?
Although genetically caused hair loss (Androgenetic Alopecia) is predetermined to a great extent, you can do much to reduce other forms or retard progress:
- Maintain a Healthy, Balanced Diet: Essential for hair health in general.
- Be Kind to Your Hair: Evade tight hairstyles, rough chemicals, and excessive heat.
- Reduce Stress: Develop healthy coping skills.
- Treat Underlying Illnesses: Early treatment of thyroid disorders, infections, or deficiencies.
- Review Medications: If you have reason to believe a drug is triggering hair loss, speak with your doctor (do not discontinue medication without consultation).
- Avoid Smoking: Some research indicates that smoking has been implicated as a potential factor in the risk for Androgenetic Alopecia.
The Emotional Side of Hair Loss: Alopecia
It is essential to note that alopecia hair loss can have a great effect on emotional well-being. Anxiety, depression, low self-esteem, embarrassment, and withdrawal from social contact are usual. Hair is frequently linked to cultural definitions of beauty and youth.
If hair loss is impacting your mental health:
- Seek Support: Discuss with friends, family, or support groups (online or face-to-face) for individuals suffering from hair loss. Exchanging experiences can be extremely validating.
- Focus on What You Can Control: This could be researching treatment, experimenting with cosmetic solutions, or concentrating on other areas of your health and well-being.
- Consider Counseling: A therapist can offer coping mechanisms and assist in working through the emotional aftermath.
- Educate Yourself: Knowing your particular type of alopecia can empower you.
Moving Forward with Hope
It can be lonely, but remember that it’s a common problem with many causes and more ways to manage it every day. There are ways to move forward once you know what the problem is and have tried treatments like minoxidil, finasteride, PRP, or hair transplantation. Cosmetics and changes to your lifestyle can also help.
The most important thing to do is to talk to a dermatologist. They will be able to help you understand the details of your case, give you personalized advice, and give you realistic hopes. Not all hair loss can be fixed, but many can be treated or managed, which will help you feel more confident and hopeful about the future.